Our Miles Towards Mission
We're walking to power more research, enable more advocacy and fund more support for the 1.45 million Americans living with T1D.
Leaderboard
Participant Participants
Loading ...
Loading ...
Team Teams
Loading ...
Loading ...
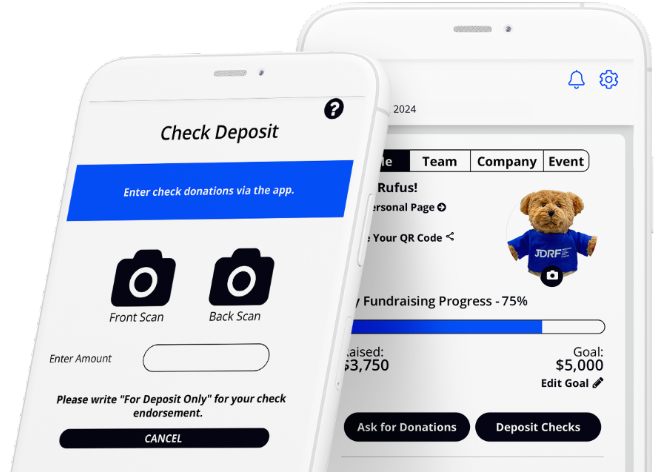
Raise more for T1D research with the JDRF One Walk App.
Fundraising is easier than ever with our NEW mobile app. Share your story and connect with more donors through text, email and social media. Deposit checks and monitor your fundraising progress on the go! You’ll reach your goal in no time!